
In July of 2018, after a string of false starts and dead ends, Chris White was finally diagnosed with mucosal melanoma, a rare subtype of melanoma that forms on ‘wet tissues’ in the body. Mucosal melanoma accounts for about 1% of all melanoma diagnosis and can affect the nasal cavity, lining of sinuses and mouth, the GI tract, vagina, anus, and other areas. Due to its rarity, its symptoms are often overlooked and misdiagnosed.
Earlier that year Chris had started to notice symptoms of what he assumed was a hemorrhoid.
While he knew he should have it checked out by a doctor, life was busy and he assumed it would eventually resolve itself. It wasn’t until he also noticed a growing lump in his groin that he made an appointment to see his doctor.
“My doctor gave me some antibiotics and told me to get back in touch if it didn’t resolve in ten days,” remembers Chris. After the first and second round of antibiotics produced no change, Chris’ doctor referred him to a surgeon for additional testing.
“The surgeon was upfront, he explained that the hemorrhoid wasn’t connected at all to my groin issue and he referred me to a different specialist for that,” says Chris. “He further explained that if the lump was a hernia, he’d fix it. If it wasn’t a hernia, he’d biopsy it and send it to pathology. Either way, I’d get some answers.”
A few days later Chris learned that he didn’t have a hernia and that he’d find out more from the pathology report in a few days. Around the same time, Chris also had an appointment with Dr. Hughes, a proctologist, to discuss the stubborn hemorrhoid.
The exam was brief. The doctor knew on sight that he wasn’t looking at a hemorrhoid. He asked Chris if he had the pathology results from his earlier biopsy.
“I was surprised and asked him how they were related, because in my head, these were two completely different health issues. He told me that he thought it might be cancer,“ says Chris.
The next day his surgeon called with results from his biopsy. The diagnosis? Metastatic mucosal melanoma.
“I found myself crying in the shower. I completely broke down,” remembers Chris. “People get cancer all the time, but I never thought it would be me – especially at just 36 years old.”
The next week he had his first appointment with his oncologist. His Mom, Dad, and two siblings came with him to provide support. During his appointment, they went over his pathology report and discussed next steps. It was during this appointment that he heard the word ‘rare’ uttered for the first time. Due to the rarity of mucosal melanoma, he was referred to the University of Texas, MD Anderson Cancer Center.
Getting a second opinion before starting your treatment is highly recommended for all patients with advanced melanoma. This is especially true for patients with rare melanoma subtypes, because many doctors will have little if any experience treating these rare conditions and won’t be up to date on the latest discoveries or available clinical trials. Learn more about getting a second opinion for melanoma.
Before his first visit at MD Anderson, Chris underwent surgery to remove the primary tumor from his rectum. The surgery was successful with clear margins.
Days later, Chris and his family made their way to MD Anderson for his first visit with Dr. Adi Diab. Dr. Diab, an expert in mucosal melanoma, explained that mucosal melanoma “is melanoma where the sun doesn’t shine” and that it forms on mucosal membranes throughout the body. He further explained that no strict standard of care exists for this rare melanoma subtype, but that immunotherapies are showing promise.
Before beginning any treatment, Dr. Diab wanted to better understand how much melanoma had invaded Chris’ body. In addition to a variety of scans, he also ordered a Sentinel Lymph Node Biopsy (SLNB) to determine if melanoma cells had spread beyond its site of origin to the nearest lymph nodes. In addition to finding some residual melanoma cells on his rectum, Dr. Diab also determined that Chris’ melanoma was already exhibiting signs of being aggressive.
To treat the residual melanoma cells, Dr. Diab suggested targeted radiation therapy to the region. “He explained that radiation therapy would destroy any chances of me having kids naturally, so I also underwent sperm banking so that I’d have options later,” says Chris.
By late November, despite the surgery and radiation, scans continued to show new lumps forming throughout Chris’ groin region. He now had Stage 4 melanoma, meaning that his melanoma had spread throughout this body including his lungs, liver, and other organs. Fortunately, his brain continued to show no signs of metastasis.
Dr. Diab suggested aggressive treatment with Opdivo + Yervoy, a combination of two checkpoint immunotherapies that help unleash the immune system against melanoma cells in two different ways.
While his care was managed at MD Anderson by Dr. Diab, Chris was able to receive his infusions at a local facility in Dallas. “This really did make it easier for me and my family,” remembers Chris.
“I didn’t have a clue what was going to happen, but I kept telling myself, as long as I keep at it – keep living – melanoma won’t beat me,” says Chris. “I don’t have my own family – no real legacy of my own – so I decided that my legacy was that if melanoma was going to take me – I’d go out swinging.”

After two infusions of Opdivo + Yervoy, Chris was back at MD Anderson for scans in January. Thankfully, his brain still showed no metastases, but his response to the therapy was mixed.
Dr. Diab was concerned that the melanoma was growing too fast. He recommended trying to slow it down with a chemotherapy combination called CVD, which is made up of the three medicines: cisplatin, vinblastine and dacarbazine.
While chemotherapy is usually not used to treat cutaneous melanoma, the most common type of melanoma that forms on sun-exposed skin, it is still an important treatment option for patients with mucosal melanoma.
Two cycles into this new regimen, scans revealed slight tumor shrinkage. However, it wasn’t working as well as Dr. Diab had hoped, so he suggested another dose of radiation.
After the third round of chemotherapy, Chris switched back to combination immunotherapy and restarted Opdivo + Yervoy on March 11. Under the direction of MD Anderson’s Dr. James Welsh, Chris also underwent a series of intensive radiation treatments in-between his immunotherapy infusion cycles.
At this point in Chris’ journey with melanoma, things started to look up. His eyelashes started to bleach with vitiligo, a sign that his immune system was attacking melanocytes – in addition to the melanoma cells – throughout his body. While stressful for many people, vitiligo is actually associated with prolonged survival among patients with melanoma treated with checkpoint immunotherapies.1
However, the repeated rounds of combination immunotherapy were starting to take their toll on Chris’ body. He developed stubborn colitis, a common immune related side effect, and started to shed weight.
By May, the colitis had become severe, and he began high dose steroids to reduce his immune activation. This means that his melanoma treatment would be delayed until his side effects were under control.
“Each time we tried to taper down my steroid dosage, I’d have a relapse and the colitis would be back,” says Chris. “Colitis was a rollercoaster.”
By June, Chris was hospitalized. In July, a port was installed to allow him to receive his nutrition intravenously so he wouldn’t starve. Finally, his body began to stabilize.
He restarted his melanoma therapy in August with a new chemotherapy agent, Abraxane. “Out of everything that I’d gone through, this was the one that hit me hardest,” remembers Chris.
In October, Chris was once again sitting in Dr. Diab’s office discussing two different treatment options. He could combine the checkpoint immunotherapy Keytruda with Ibrance, a new chemotherapy drug often used in breast cancer, or he could try to enroll into a clinical trial testing an experimental TIL therapy.
TILs, or tumor-infiltrating lymphocytes, are the white blood cells that have successfully fought their way into a tumor. TIL therapy works by harvesting TILs from a patient’s tumor, expanding their numbers greatly in a lab, and then administering these lab-grown TILs back into the patient’s body. These infused cells, already primed to successfully swarm the cancer, are then further activated with high-dose interleukin-2 (IL-2).
Chris chose the TIL clinical trial.
“I just knew that I couldn’t continue doing the same things over and over again expecting a different result,” says Chris. “Previous cohorts of patients who enrolled in the study were doing well, far better than expected for patients on the second or third line of therapy. That gave me some much needed hope for my future.”

The only problem with the clinical trial: It wasn’t being offered anymore at MD Anderson. To participate, he’d have to relocate his care at a participating site. So, early the next month he travelled to the University of Colorado to learn more about the trial, provide his informed consent to participate, and begin the required eligibility testing. The process was moving smoothly, and he was quickly scheduled for surgery to extract tumor tissue needed to create his personalized TIL therapy.
The final scans needed before he was to receive his TIL therapy infusion revealed bad news: a 1 cm tumor had developed in his brain’s occipital lobe. This news, while shocking and disappointing, also made him ineligible for the clinical trial. The only way to regain eligibility was to treat and stabilize the tumor before the trial wrapped up enrolling new patients, a window of time just weeks away.
“Everything felt like it was moving in the right direction, and then this just completely sidelined me,” says Chris. “I was told that I should start settling my affairs and to start thinking about hospice.”
Chris and his care team weren’t ready to give up. He needed to have a clear brain scan and to formally reenter the trial by December 24. That deadline left them days.
He received insurance approval for more targeted radiation therapy on December 16, was fitted with a custom mask to stabilize his head into position on December 17, and then received five stereotactic radiosurgery (SRS) treatments over the next four days.
“Every day during this period, I was in bed and my family would take turns sitting with me,” recalls Chris. “We were all just waiting to see what would happen next. It was surreal.”
Chris made the cut. He became the last patient dosed as part of the clinical trial.
One month later, scans showed that all of his tumors were shrinking. In fact, the tumors on his lung and liver were already 50% smaller. “I describe mucosal melanoma as an assassin, slowly following me,” says Chris. “So, when I heard the scan results, for the first time in forever, I felt free.”
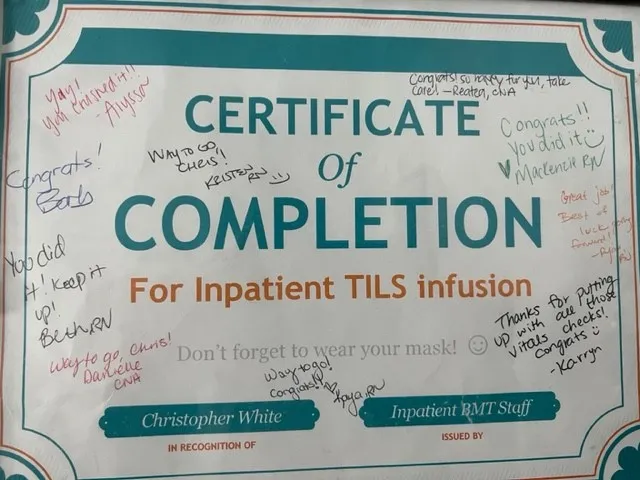
Over the following months, his scans continued to show improvement. He started physical therapy, had his port removed, and started to think about his future. “I realized that the stunned, paralyzed feeling of being chased by melanoma was gone.”
Today, over a year since Chris received TIL therapy, his scans continue to show no evidence of disease. He’s still recovering from the physical, financial, and emotional trauma that this has caused him, but is optimistic about his future. To help future patients with mucosal melanoma, he started the website MucosalMelanomaSurvivor.com and hopes to re-launch his career focused on patient advocacy and public speaking. “I just want other patients to know that you can beat melanoma. Don’t give up. There is a way.”

By joining MRA’s RARE Registry, you'll be joining a supportive and growing community of patients, advocates, and loved ones who are committed to advancing research into rare melanoma subtypes.
Learn More About MRA's RARE Registry
More to explore